A retrospective study
In the present study, the data of 10.165 implants at 3.095 patients from three implantologically oriented practices raised according to identical criteria and summarized.Of the patients, 55 percent were women and 45 percent men who were cared for between 1991 and 2011.The survival rates were determined with the Kaplan Meier method and as an input-output calculation and u.A.The influence of age, gender and implant type tested.
The communications for the overall survival rate of implants have developed significantly in the past 15 years.Tetsch (1977) reported by failures of the size of 50 percent.1 Die Deutsche Gesellschaft für Implantologie (DGI) ging 2000 davon aus, dass nach zehn Jahren, je nach Indikation und Versorgungsart, zwischen 71 und 97 Prozent der Implantate unter Funktion stehen.4 Seitdem tendieren die Aussagen eher gegen 95 Prozent.5–9 Es konnte gezeigt werden, dass zu dem zeitlichen Erscheinen der Artikel auch der Umfang der Untersuchung und deren Beobachtungsdauer eine Rolle spielt.2 Je jünger die Publikation, je länger die Beobachtungsdauer und je mehr Implantate eingeschlossen waren, desto günstiger waren die Resultate, obwohl kaum eine Publikation die Bedeutung der individuellen Erfahrung der Operateure/Prothetiker berücksichtigt.
The study by Jemt et al is an exception.2016, in which the relationship between the success rate and the surgeons could be shown.10 Auch die Deutsche Gesellschaft für Orale Implantologie e.V.(Dgoi) in her scientific evaluations to risks and complications indicates that success and failure obviously crucy of the expertise or.The operator's learning curve and the expert use of the latest technical developments in implantology depend.11
Temmerman et al.on the other hand, in 2015 that guided students produce similar success rates as experienced implantologists.12 Eine ähnliche Ansicht vertraten Kroeplin und Strub 2011.13 Die meisten Implantatverluste treten in der Phase der Einheilung bzw.in the first year, further losses are then distributed over the next 20 years.Lemmermann and Lemmermann gave in 2005 at 1.003 implants that 75 percent of the losses occur in the early phase.14 Hauptverlustursachen sind initial die nicht erfolgte Osseointegration, später die Periimplatitis, Überlastungserscheinungen und Brüche.In this study, the total survival rates in particular should be considered depending on the experience of the surgeons and the implant types.
Galerie
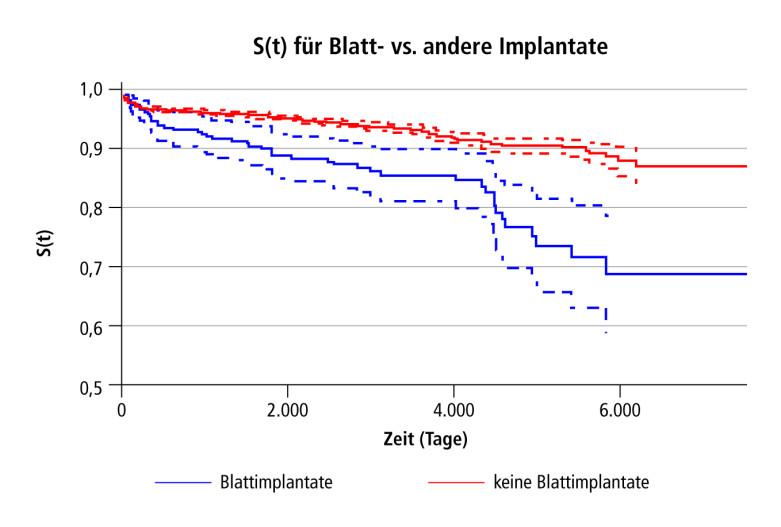
Abb. 1: Überlebenswahrscheinlichkeit aller Implantate. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 2: Überlebenswahrscheinlichkeit nach Implantatarten getrennt. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 3: Patientenbezogene Überlebenswahrscheinlichkeit der Blattimplantate. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 4: Überlebenswahrscheinlichkeit nach den Patienten ohne Blätter. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 5: Implantatverluste in Abhängigkeit von der Liegedauer. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 6: Implantatfrequenz der Behandler pro Jahr. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 7: Implantatverlustquoten nach fünf Jahren Liegezeit. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 8th: Implantatverlustquoten nach zehn Jahren Liegezeit. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 9: Überlebenswahrscheinlichkeit 2001 bis 2011. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 10: Überlebenswahrscheinlichkeit in den beteiligten Praxen 2001 bis 2011. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 11: Überlebenswahrscheinlichkeiten der Astra-, CAMLOG- und Friadent-Implantate 2001 bis 2011. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 12: Überlebenswahrscheinlichkeiten der Blatt-, Pitt-Easy- und ZL-Implantate2001 bis 2011. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 13: Darstellung der Überlebenskurven nach Kaplan-Meier unter Berücksichtigung der angenäherten Implantatoberfläche (umschreibender Zylinder), die kurzen und dünnen Implantate (grün) haben anfänglich höhere Verluste. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai SchmengerAbb. 14: Überlebenskurven nach der Indikationsklasse 2001 bis 2011. © Dr. med. habil. Wolfram Knöfler, Dr. med. Thomas Barth, Dr. med. Reinhard Graul, Dr.Dietmar Krampe, Dipl.-Biol.Kai Schmengermaterial and methods
All patients who were provided with implants between August 1991 and December 2011 were included in their own observations between August 1991 and December 2011.A total of 3.095 patients 10.165 implants advertised.Table 1 shows an overview of the implant types used.Of these patients were 1.693 women (55.3 percent) with a total of 5.626 implants and 1.401 men (44.7 percent) with 4.539 implants.In a patient, no information about gender was given.
The middle age of the patient at the time of implantation was 52.4 years.On average, 3.32 in women, and 3.24 implants were advertised for men.Compared to an earlier message, the patients are now four years older and have an implant more.15
parameter
In addition to demographic data, the following parameters were collected:
Implant type, length, diameter, position, indication class (single tooth replacement [EZE], tooth group replacement [ZGE], reduced residual dentition, toothless [Zuk, Zok], "repair implants" [PVRep]), time of implantation, day of opening, daythe integration of the supracon structure, type of superstructure, augmentation type, complications, day of the implant loss, cause of loss, day of last control.
The data material was recorded in tables and statistically processed with regard to the individual questions.
Statistical methods
The statistical calculations were used using SPSS 11.0.0 (IBM, Armonk, NY, USA) and using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA) carried out.Depending on the question, the following parameters were given as part of the present analyzes:
Significances in the individual subgroups were determined using log-rank or chi square test statistics.The P values and test statistics are reported.In the case of statistically significant group differences, the estimated difference (percent) and its 95 percent confidence interval are given.
Results
The implant -related survival rate and probability
The one-year survival probability of all implants was 97 percent, sank to 96 percent after five years and after ten years to 93 percent.After 16 years, the length of stay was likely to be 8th6 percent (Fig.1).
The total loss rate (loss rate) of 4.54 percentages determined to 4.20 percent if the 28th0 leaf implants are not taken into account.There are hardly any leaf implants today or.can no longer be used, a course of the length of stay is more likely to assume, as is shown by the red curve in Figure 2.
After that, the probability of survival of the rotation -symmetrical implants is around 8th8th percent after 16 to 20 years, which of the leaf implants at 70 percent (Fig..2).
The patient -related survival rate and probability as a whole
If one looks at the patient-related probability of survival, which includes the loss of an implant in a patient is the observed event, a remarkably lower course of the Kaplan Meier curve can be seen and expected (Fig..3und4).This means that patients who have been carrying rotation -symmetrical implants for 20 years have met 30 percent of a loss event, and with leaf implants it was even 40 percent.In the first two years 1991/92, the result was significantly influenced by ZL-Duraplant implants and leaf implants (S.U.).200 days led.Without this it can be assumed that a loss event would only occur in the patient's 15 percent.
Loss of implant causes
A total of 10 years went from 10 years from 20 years.165 advertised implants lost 461, which is 4.54 percent.For the individual practices, the values were 3.7 percent (Praxis Barth), 4.58th percent (practice gray) and 5.62 percent (Praxis Knöfler).If you look at the results without leaf implants that initially played a certain role, the numbers were 3.7 percent, 4.46 percent and 4.8th8th percent.The reasons for the explantation were mainly acute and chronic peri -implantitids, whereby the classic peri -implantitis dominated with soft tissue division and bone infestation (tab.2).In the guidelines or statements of the leading scientific societies, the late form of peri -implantitis with mucositis and ostitis is used, referred to by the authors in the article as peri -implantitis chronica.17.18th
The early forms of inflammatory phenomena, which also lead to loss, are less taken into account.These are the acute osteomyelitis or their locally limited form, which immediately force the implant (peri -implantitis totalis acuta), or the gradually running form that does not stand out to the patient and is also not surprisingly determined by the practitioner and at the opening that none is foundOsseointegration has taken place, but the implant crows (peri -implantitis totalis chronica).From a pathohistologically point of view, this is also very good, although they go completely different from the later peri -implantitis with mucositis and progressive bone loss around the implants after initially Osseointegration (teaching content at the University of Leipzig, DR.Hans-Ludwig Graf, personal message).
Most of the implant losses occurred during the healing time in the first few months of up to two years.In the first six months, 174 implants were lost, another 90, up to five years, another 69, up to 15 years 114 and then six (Fig..5).
Only eight implants were lost due to the implant broken. Das waren ein Semados®-Implantat (3,8th x 15 mm) bei 46, eine Brånemark-Fixture (3,5 x 15 mm) bei 23 (Brücke bis 28th), ein Astra-MicroThread-Implantat (3,5 x 9 mm) bei 36, zwei IMZ-Zylinder TwinPlus (3,3 x 15/13 mm) bei 13 und 17, ein ZL-Implantat (2,9 x 15 mm) bei 23 und zwei Blattimplantate bei 15 und 16.
Iatrogenic influencing factors: learning curves of the practitioners
It can be assumed that every practitioner has a few more problems when familiarizing it into a new field of activity than the veteran.Examining this was a tempting option in this data material.

After the first, rather tasting attempts, the procedure became more routinely in the following years and achieved a temporary maximum after 14 years (Fig.6) With almost 1.000 implants per year.
The further investigation was divided into steps of two years because the implant number in the practices was initially too low than that an annual consideration would have been worthwhile.
In 1991/92, 70 implants were advertised (TIOLOX15, two Explaned in five years, Blätter 19/5, ZL 14/2 and IMZ 22/0).After five years of lay period, nine of these 70 implants were lost (12.9 percent), after ten years it was one more (14.3 percent).
In 1993/94, 233 implants were advertised, after five years 13 (5.6 percent) and after ten years 16 (6.9 percent) were explained (Blätter 62/6, ZL 90/10, Tiolox, Frialit II, IMZ,K.S.I.Bauer-Schläube GmbH and Biolox no losses).
Of the 28th1 implants in 1995/96, after five years 26 (9.25 percent) and another five were lost after ten years, 31 (11.3 percent).
In 1997/98th there were 509 implants that had 48th (9.4 percent) losses after five years 35 (6.9 percent) and ten years.
1999/2000 were 28th (3.4 percent) and 46 (5.51 percent) of 8th35.
The consideration for ten years of lying time had to be ended, since the observation was completed at the end of 2011 and therefore less than ten years were achieved.However, the consideration after five years of lounger could still be continued.So the survival rate of the 1 was.210 implants from 2001/02 at 5.3 percent, the 1.553 of 2003/04 at 2.5 percent and the 1.8th33 implants from 2005/06 at 3.1 percent (ABB.7 and 8th).
On closer inspection, it turned out that the initially so high losses were mainly due to the leaf implants (26 percent after five years) and the ZL-Duraplant implants (21 percent), both of which were intended for reduced bone offer while avoiding augmentation.With more experience, this was better (1993/94, leaves 9.7 percent, ZL 11 percent after five years), but remained significantly behind the other implants used, which had no losses. 1995/96 wurden zusätzliche Implantattypen eingeführt, die sofort hohe Verluste nach sich zogen, Brånemark 10/4 (40 Prozent), Semados® 6/3 (50 Prozent) und noch immer Blätter 34/6 (17,6 Prozent) und ZL 7/2 28th,6 Prozent.In 1997/99 it was 22.5 percent losses for leaves and 15.4 percent at ZL.In 1999/2000 the Camlog implants were added and after five years recorded 12.3 percent loss, which never occurred again so high.Already in the following year it was only 3.3 percent.So it seems to be the case that the introduction of a new system initially brings some starting difficulties that can express themselves in the survival rate.
The patient -related survival rate and probability 2001–2011
In order to enable a consideration that assumes that the implants are used by an already experienced surgeon, the entire statistics were expected again, but only the period from 2001 to 2011 was taken into account.This calculation then went 8th.230 implants and the loss rate was only 3.28th percent.The Kaplan Meier curve ends around 95 percent after ten years (ABB.9).Leaf implants only play a very subordinate role and only influence the final result by 0.03 percent.
The loss rates of the individual practices were now 2.8th1 percent, practice Graul 4.03 percent and practice Knöfler 3.77 percent.Figure 10 shows the corresponding Kaplan-Meier curves.
The implant types used since 2001 achieve a level of survival of well over 90 percent, and even the 98th leaf implants advertised with corresponding experience are still 90 percent in sit.11 and 12).
With regard to the expectation of success in the upper and lower jaws, there were no other results compared to the overall sample (see.Knöfler 2016).2 The losses in the upper jaw were significantly below those of the lower jaw (2.57 to 4.09 percent).This also met the individual tooth group positions.The difference in the augmented camp (lateral jaw collecting crested stations, internal and external single-sized sinus lift socks) advertised implants to those in the local bone remained significant (augmented: 2.96 percent, not augmented: 3.8th3 percent, p = 0.0313) (tab.3 and 4;see.Knöfler 2016).3 The log-rank test for the time course no longer confirmed this (p = 0.068th4; cf..Knöfler 2016).3
The gender -specific survival rate was significantly higher for women.The implant dimensions still had the same influence that thinner and shorter implants were disadvantaged according to the loss rates (Tab.5 and 6;Fig.13;see.Knöfler 2016).19
There were no more differences between the indication types (Fig.14).The single crown remained the most successful supply in terms of survival curve (p = 0.0001) compared to all other types of supply.
Summary
The implant -related overall survival rate of all implants in this retrospective study achieved a value of around 8th6 percent after 16 years, and since no further implant was lost, this also applies to the period of 20 years.
The loss rate of rotary symmetrical implants was 4.20 percent after 20 years, the final values of the Kaplan-Meier curve 8th8th percent.For the leaf implants, the curve ends at 70 percent.
The patient -related consideration suggested that after 20 years in about 30 percent of patients with rotation -symmetrical implants, a loss event occurs, mostly without impairing the functionality of the dentures.
Half of the lost implants had not healed in the early phase, the other half was lost by chronic peri -implantitis.Only eight implants broke.
The learning curve of the surgeons and the implants used at the respective time had a decisive influence on the end result.While in the western federal states the implants had played an increasing role since the 1960s and the dentists have grown with implantology, so to speak, the start after the political turnaround in 198th9 in the new federal states was a synchronizing event, which is why the learning curve was particularly clear.In the first few years of observation, the loss rate in the practices involved decreased steadily and was 5 percent after ten years and below.Tetsch had assumed failures in 1977 from up to 50 percent within five years.1 Eine Analyse der Resultate aus der Zeit von 2001 bis 2011, 8th.Comprehensive 230 implants, only 3.28th percent have losses.The Kaplan Meier analysis ends at around 95 percent.
Even between the then many implant types that were used, there are no more differences.However, the differences between the upper jaw and lower jaw and between the augmented implants and those in the local bone had remained.2,3 Implantate im Oberkiefer und im augmentierten Lager hatten signifikant höhere Überlebenswerte.
In summary, it can be stated that, according to the appropriate experience of the implantologists, the survival rate of the implants is leveled in about 95 percent after ten years, whereby certain deviations are caused by the implant types used, the indication and augmentation.
discussion
In the investigations, the implant-oriented survival period of the rotation-symmetrical implants was determined with 8th8th percent after 20 years, the leaf implants used earlier with 70 percent at the end of the Kaplan-Meier survival curve (Fig..2).If, on the other hand, one examines how many patients who have been wearing implants for 20 years (and are still under control!). A loss event has occurred, this is the case in 30 percent of these patients, although this concerns only 12 percent of the implants itself, this iswhich are still under observation and only 4.2 percent according to the loss rate.Would all of their own patients be under observation, what due to death, move, etc..cannot be reached, the number would rather approach the lower values.
Derks et al.2015 state that of 2.765 patients with 11.311 implants were ultimately published for the follow -up examination after nine years and of which 4.4 percent early losses (preprothic) were.Further 2 percent of the implants were lost later.Derks et al.further state that only 7.6 percent of the patients had suffered at least one loss event, but could also be used for the not published about 9.500 implants do not make a statement.20
If one compares the number of explantations (loss rates) in the number of prosthetically supplied implants, this results in a value of 2.56 percent loss after 20 years.Studies with only one implant type give 96.7 percent for ITI implants, for 1.554 Frialit-2 implants a probability of survival of 94.8th percent after seven years and for 12.736 Ankylos implants 93.3 percent after 17 years.5.6.8th
For all implants, a relatively high loss rate in the healing time is up to six months.The postprothetic loss rate, on the other hand, is very low.Only eight breaks were observed.These implants stood in stress -intensive positions and also served as a bridge pillar, which increases the load.The dimensioning of the implants at these positions may be described as insufficient at ≤ 3.5 mm.On the other hand, Krebs et al.2013 that 3.5 mm ankylos implants can be successful at all positions-it will probably be important in the end of the construction of the implants.8th
It can also be assumed that the loss rates are better off with limited indication than with implantation in the entire width of the possibilities.So it also seems to be justified to tell that inexperienced good results can achieve.13,14 Die Autoren hingegen mussten feststellen, dass die Fehlerraten zum Beginn der implantologischen Tätigkeit durchaus deutlich höher ausfielen.If the first phase of familiarization into the area of implantology is overcome, the loss rate becomes significantly lower.The implant types used had a clear influence.Leaf implants that the authors still used because there were simply no surgery units before the turn in the GDR that would have been able to.B.Using a 3.5 mm spiral drill in the bone, but very well a lindemann milling, had high loss rates as well as the ZL-Duraplant implants constructed for atrophied, narrow bone areas (2.9–3.5 mm diameter)).The evaluation of the period since 2001 leads to significantly different results compared to 1991 to 2001.Now the loss rate was, for example, 4 percent after ten years and the Kaplan-Meier survival rate occurred in about 95 percent.There is no longer any difference between the indication classes (p = 0.329). Zwischen augmentierten und nicht augmentierten Implantaten verschwindet der Unterschied ebenfalls (p = 0,068th4), obwohl noch immer ein gewisser Trend zugunsten der augmentierten Implantate festzustellen war.The upper jaw, on the other hand, remained advised (p = 0.0001). Bei den Implantattypen lautet die Reihenfolge Astra (0 Prozent Verlust), CAMLOG (1,56 Prozent Verlust), Friadent-Produkte (1,8th6 Prozent Verlust) und andere (4,26 Prozent Verlust) ohne signifikante Unterschiede.
Die patientenbezogene Überlebenswahrscheinlichkeit der Implantate liegt nach zehn Jahren bei etwa 8th0 Prozent, d.H.With every fifth implant, a loss event can be expected.
Overall, it can be assumed that the learning curve has an impact on the probability of success of the implants.In view of the long observation period, it must also be considered that implants were used at the beginning of the activity that are no longer available on the market today.In addition to the experience of the practitioners, the corresponding further developments in implant design and surface finishing should also contribute to improving the survival rates.
Summary
Your own results have shown that Learning by doing brings an increase in experience, which leads to better accumulation when structured further training and practical courses accompany this.Consequently.V.(Mvzi) installed.This path was successfully carried out by the German Society for Dental Implantology E.V.(DGZI), the German Society for Implantology (DGI), the German Center for Oral Implantology E.V.(Dzoi), the Federal Association of Implantologically active dentists in Europe (BDZI EDI) U.A.continued and undoubtedly led to the considerable progress in implantology.Based on our own experiences, we recommend that such an advanced training path and favorite also to spend the time of assistance in an implantologically oriented practice, which enables the daily exercise and correction.
More authors: Dr.Dietmar Krampe, Dipl.-Biol.Kai Schmenger
The full list of literature is available here.
The specialist contribution has been published in the Implantology Journal.
Photo: Talaj - Stock.Adobe.com










Test winner at Stiftung Warentest:...
How to get the perfect look for Cos...
Dry elbows: This is how brittle ski...
Cream for Rosacea: The Best Creams