More than 100 implant systems are offered in Germany alone. And with every IDS there are more. Not only the surface, the design and the variety of structures form quality and distinguishing features, but also biomechanical aspects. How do you find the right system? The current circle of experts offers decision-making aids.
The requirements for an implant-abutment connection are diverse. It must be tight under chewing function load, meet the necessary strength requirements and keep the stresses on the bone as low as possible in order to have a favorable effect on the remodeling. In addition, handling should be as simple as possible.
Is there an "ideal" implant-abutment connection?
Von See: There are currently a number of good systems that enable a competent frictional connection between the implant and the abutment. However, I see a long-term problem in the biological interaction between the internal connection on the one hand and the hard and soft tissue on the other. This does not seem to be understood in detail, let alone solved in an “ideal” way.
Abramowski: Ultimately, implantologists or prosthodontists make their choice based on individual preferences, handiness and simplicity of their system.
What role does the indication play?
Günther: It can of course contribute to the decision, just like the insertion office. However, a good implant-abutment connection can be used in any region for any indication.
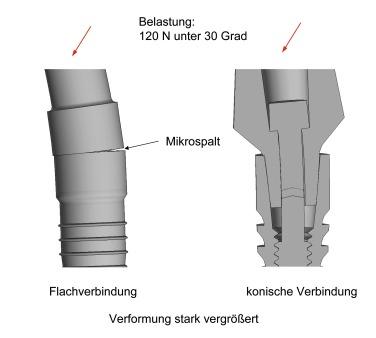
Three connection types can be distinguished: Flat connections such as standard external hex connections, heavily conical connections with cone angles < 15 degrees and medium conical connections with a cone angle of approximately 45 degrees.
Do you have a favorite?
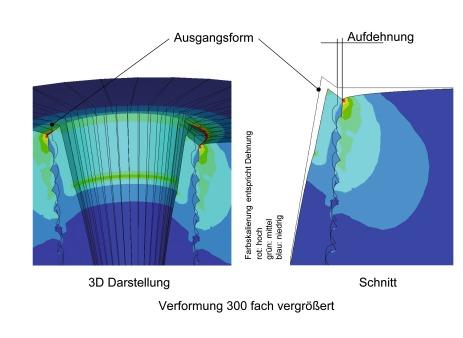
Stretchbein junior: For me, medium conical implant-abutment connections with 45-degree cone angles are currently the best. This connection can reduce the two relevant parameters microgap and bone load to a physiological level. The results of our joint investigation with the Koblenz University of Applied Sciences with regard to these parameters have recently been published in the Journal of Dental Research.
Please characterize the main connection types according to biomechanical criteria.
Flat: Strongly conical connections do not show a micro-gap under masticatory forces (Fig. 10), but due to the wedge effect of the cone, they lead to additional stresses in the implant during loading, which can be transferred to the bone if the wall thickness of the implant is small ( Fig. 8, 9, 11).
When does this wedge effect become noticeable?
Flat: Especially with implants in the diameter range ≤ 4 mm. This is due to the usually low wall thickness of such implants.
What can help?
Flat: Medium conical connections. They combine the favorable properties of the flat connection with those of the strongly conical connection:
Not only the right connection has an influence on the primary stability, but also the thread design. What are the criteria in this context?
Streckbein senior: Unfortunately, there is a lot of semantic uncertainty regarding the respective effect of different screw designs on their environment. A distinction is made between self-tapping, non-chip-removing screws (self-condensing) and self-tapping, chip-removing screws. However, these nuances in design are not as important as the magnitude of the pre-drilling. This pre-drilling mainly determines whether good stability can be achieved with reasonable torques. If you look at the conical, screw-shaped implants that are favored today under these conditions, you will see by analogy that a slightly larger pre-drilled hole is made for the self-tapping insertion of a non-cutting implant shape than for the self-tapping insertion of a cutting implant shape. The difference in the bony implant bed results from the fact that with the non-cutting thread form the bone is slightly displaced laterally, while with the cutting form it is cut out of the bed during the screwing-in process and embedded in the groove, as is known with thread cutters. However, this bone, which has been completely detached from its surroundings, usually heals again as part of the remodeling.
That sounds complicated.
Streckbein senior: Correct – and in order not to have to go through the lengthy attributes that the standardization manuals for screws require every time, the dental market describes both thread nuances as self-tapping and by that means only the clinically relevant main feature, namely that these implants can be used in many Cases can be used without pre-cutting using a tap.
When are self-tapping implants indicated?
Stretchbein senior: In principle, all self-tapping implants are advantageous in terms of stability, for example in the case of immediate implantation. For cases with only cortical bearing bone portions, all leading implant systems also offer taps to prepare the bearing accordingly and to keep the torques under control during implantation.
Will they prevail in the long run?
Von See: Yes, because these offer the possibility of strengthening the primary stability in soft bone and at the same time – with higher bone density – avoiding bone compression by pre-cutting a thread. From my point of view, the preparation of the implant bed is much more important. This topic still raises many questions with regard to bone quality and the resulting osseointegration processes. In short: an implant with a thread design that can be used for every indication would be ideal.
Dr. Günther, which thread design do you think has the best future?
Günther: The trend is clearly towards self-tapping and root-forming. However, the implants should not taper too much, i.e. have a medium cone angle, I agree with my colleagues. A number of providers have introduced these types of implants in recent years or are doing so at the moment.
But German dentists are still advertising parallel-walled implants - and not too little.
Günther: That's right - mostly in Germany.
So parallel-walled implants are "out" abroad?
Günther: More or less, in any case there is a clear trend towards root-shaped systems.
What other criteria are important?
Günther: With a root-shaped design, the tip of the implant must be rounded, otherwise there is a risk of injury to anatomical structures, e.g. B. the Schneiderian membrane or the nerves. I think an additional integrated platform switching is important, because it offers demonstrable advantages in preserving the crestal bone. I prefer variable macro and microstructures for the implant surface.
Even on the implant shoulders?
Günther: Here I prefer rough, unpolished surfaces and a continuous thread. This means that an implant can be used with a simultaneous external sinus lift even if there is minimal bone availability. In the apical area, a system should be rather rough with a strong thread; in the area of the implant shoulder, a less rough and less strong thread shape shows advantages in peri-implantitis.
It is said that a thread design should be based on the requirements of the bone. Which biomechanical criteria are particularly important in this context?
Flat: The strength of the implant and the bone stress can be significantly improved by bionically and thus biomechanically designed threads.
Please specify.
Flat: In the area of microthreads, bone stress can be reduced by up to 30 percent or more with a bionic thread structure, i.e. a thread structure designed according to the growth laws of nature. But not all microthreads are the same. And: From a biomechanical point of view, the design of the microthread is more important than the much-discussed platform switching.
What do you mean - the importance of platform switching seems to be universally accepted...
Flach: That's right, but the platform-switching discussion fails to take into account that the impact can only be achieved directly at the level of the platform-switching stage. But if the bone is only half a millimeter below this level - and this is not uncommon - platform switching is biomechanically ineffective.
Bionic microthreads are much more flexible here. The biomechanically favorable effect is possible over the entire microthread. In my opinion, the thread design that optimally meets the requirements of biomechanics will prevail in the long term.
Does this require a new study design?
Flat: Definitely. In order to proceed further along this path, the clinical studies on bone remodeling must also include information on the biomechanical parameters important for bone remodeling. To do this, you need to know the biomechanical influencing factors. Ideally, these should also be taken into account quantitatively in the study design. There are powerful methods for this, but they have so far been lacking in medical and dental education.
How can this be changed?
Flach: Only through interdisciplinary cooperation between medicine and engineering. Previous clinical studies on bone remodeling usually only refer to the microgap and biological width, but not to the biomechanical bone stress.
What are the consequences of this?
Flach: There may be misinterpretations of the study results.
Keyword immediate implantation - as is well known, sufficient primary stability and freedom from infection are decisive for success here. Which implant types or which thread design do you recommend?
Stretchbein senior: These are conical, non-cutting implants. My current ideas regarding the healing modes in the bony layer are based on 30 years of implantological experience. According to this, advantages could be expected in immediate implantation if non-cutting implants are inserted in an extraction socket, since the lowermost threaded sections of an implant can usually only be brought into full contact with the bone in the apical part of an extraction socket. This roughly corresponds to the bottom 4-5 threads. The self-tapping, non-cutting insertion leads to a desirable lateral bone compaction with good primary stability. With chip-removing implants, I also see disadvantages due to the existing grooves in the apical area, e.g. For example, when only four threads can be anchored in the bearing and the implant screw parts close to the shoulder, which otherwise provide stability, have no bone contact. However, the current scientific data situation does not yet allow any reliable statements to be made (Fig. 7).
Günther: Much more important than the implant type is the indication. No type of implant can compensate for an incorrect indication. And that is attempted far too often. I'm more conservative and prefer delayed implantation, which is much more sustainable and predictable. However, if immediate implant placement makes sense, the implant should be long and have great primary stability. And: Here, too, the drilling protocol is more important than the implant type. In short: Immediate implantation is less dependent on the type of implant than on the indication and the surgical procedure.
How narrow can an implant be? This question is also currently being discussed.
Stretchbein junior: A two-part system should be used in which the implants can be blocked using bar constructions. Systems up to a reduction to 2.7 mm are commercially available here. A further reduction includes the one-piece design and thus a clear restriction of the indication.
What are the limits of diameter reduction?
Von See: Especially when it comes to loading the implant with lateral and extra‧axial forces. The digital procedures of guided implantation and the simulation of the load direction of the implant help to keep the extra-axial forces low. Personally, I think that we are currently not able to adequately simulate the precise limits of the mechanics of the interaction between the bone and the implant. I think it is premature to make final statements on this. The precise mechanical relationships are not yet understood here. This not only applies to the reduction in diameter, but also to the short implants.
Bone augmentation can often be avoided with diameter-reduced two-piece implants. They are therefore very well suited for minimally invasive treatment...
Flat: That is correct, but two-piece reduced-diameter implants pose great challenges to implant design. In the area of two-piece diameter-reduced implants, only flat connections are possible for reasons of strength. Due to the small diameter, the thread design should always be based on bionic aspects. In this way, notch stresses in the implant can be avoided and high-strength, two-part implants with a diameter of less than 3 mm can be produced. Implants with a reduced diameter are to be used advantageously in the front tooth area and in the case of splinted constructions in the atrophied jaw.
What do you say, Dr. Gunther?
Günther: For me, diameter-reduced implants are implants with a smaller diameter than approx. 3.2 mm. We only use these in our clinic as temporary implants. If the bone is too narrow, a narrow implant is the wrong way to go. For good aesthetic and functional results, we simply need sufficient bone and soft tissue. Otherwise, augmentation or appropriate bone optimization is used. I say to my patients that you don't build a house on a dilapidated foundation. Narrow implants with a diameter of 3.2 to 3.5 mm are suitable for the lateral anterior region in dentulous jaws. Otherwise, I always aim for diameters of more than 3.5 mm.
On the question of material: Titanium implants are currently the clear gold standard. But a number of manufacturers, including well-known ones, are trying to produce zirconium implants.
Do the all-ceramic variants have a future?
Stretchbein senior: Investigations into improving osseointegration could significantly improve the indication for zirconium implants. Studies on this problem have already been published (CID 2013 Pardun et al.). In addition, the implant-abutment connection is a problem area with ceramic implants that has not yet been finally optimized. At the moment I don't see any replacement of the material titanium, we will see what the future will bring.
Von See: The development of zirconium implants has progressed enormously. From a purely mechanical point of view, however, they are currently inferior to titanium implants, even if developments in the prosthetic area in particular are showing remarkable results. It remains to be seen to what extent the latest developments in the field of zirconium surfaces on implants will have a positive effect on the long-term result.
Dr. Abramowski, how do you see the future of all-ceramic implants?
Abramowski: The real breakthrough will take a while. Despite excellent osseointegration properties and excellent soft tissue compatibility, the stability under load cannot be compared with that of titanium implants. Furthermore, with one-piece zirconium implants, we have the disadvantage that incorrect positioning and insufficient soft tissue are difficult to compensate for. If a zirconium implant were in two parts and had the same mechanical stability as titanium implants, then the zirconium implant would certainly be harmless and fully marketable. Then it is the implant of the future.
Do we need further studies?
Von See: Yes, the research areas at the university should focus primarily on the mechanical principles of the interaction between bone and implant, regardless of the question of materials. Many augmentations could be avoided and the range of indications for implants expanded by improving the external geometry of the implant. I still see great potential here, especially in the area of patients with previous illnesses.
For us clinicians and practitioners, long-term predictability and clinical stability from a functional and aesthetic point of view are a necessary area of development. Here I would like to see a closer connection between university and practice.
What do you expect from the industry?
Von See: From my personal point of view, since the surface coating of implants with growth factors or other bioactive substances offers little potential, it is worth considering which options for faster and safer osseointegration are conceivable and realizable. Procedures should be tested that allow for higher mechanical stress during immediate implantation.
Summary
The Experts
Dr. Stefan Günther studied dentistry in Münster and has been working at the Dental Clinic in Essen at the Elisabeth Hospital since 2010. Since 2013, the oral surgeon has also acted as a partner and training officer. He is a reference user of various implant systems and has been an author and speaker since 2006. Contact: stefan.guenther@zahnklinik-essen.de
Dr. dr Philipp Streckbein is Senior Physician at the Clinic and Polyclinic for Oral and Maxillofacial Surgery at the University of Gießen. Together with his father, he also works at the institute for dental implantology in Limburg. His clinical and scientific focus is on dysgnathic surgery and implantology. Contact: anmeldung@izi-online.de
Dr. dr Roland StreckbeinThe former president of the German Society for Implantology (DGI) has been based in Limburg since 1978. Since 1999 he has been developing instruments and implants with the Institute for Dental Implantology, which enable reliable implant treatment even in difficult jaw conditions. Contact: anmeldung@izi-online.de
PD Dr. Constantin von Seestudied dentistry in Göttingen and has been a research associate at Hannover Medical School since 2008. Since 2008 he has published more than 50 scientific publications and is a national and international speaker. At the Hamburg dental clinic MEDECO, he heads the training center. Contact: zhha@medeco.de
Dr. Philip Abramowski M.SC. studied dentistry in Bonn and has been working in the dental clinic of the Elisabeth Hospital Essen AG since 2005, since 2008 as a partner. He is a reference user of various implant systems and is involved in dental implantology training. Contact: info@zahnklinik-essen.de
Prof. Dr.-Ing. Matthias Flach studied theoretical mechanical engineering in Siegen and received his doctorate in the field of the service life of rail vehicles. Since 2003 he has held a professorship at the Koblenz University of Applied Sciences in the engineering department for mechanics and mechatronics. Among other things, he examines the bone stress around dental implants. Contact: Flach@hs-koblenz.de










Test winner at Stiftung Warentest:...
How to get the perfect look for Cos...
Dry elbows: This is how brittle ski...
Cream for Rosacea: The Best Creams